Diagnosing Sjögren’s can be difficult, because not all Sjögren’s patients present in the same way, have the same symptoms, or are positive for all tests associated with the disease. In addition, not all Sjögren’s patients have dryness at onset. Especially in younger Sjögren’s patients, symptoms are less likely to include dryness and more likely to include parotitis, positive serologies, neurologic and nephrologic manifestations, and non-specific features such as fever and/or lymphadenopathy.1
A physician should note the many different symptoms described on this website and in other Sjögren’s Foundation materials and media that Sjögren’s patients might have and that could lead to one suspecting Sjögren’s as a diagnosis. A diagnosis of Sjögren’s should then be based on a combination of signs and symptoms.
In 2016, an international group of experts along with the Sjögren’s Foundation, established the American-European Consensus Sjögren’s Classification Criteria. This criteria was developed for Sjögren’s patient entering clinical trials and not for diagnosing patients in a clinic. Thus, diagnosis of Sjögren’s can sometimes be an “art” based on the physician’s assessment of symptoms plus objective tests.
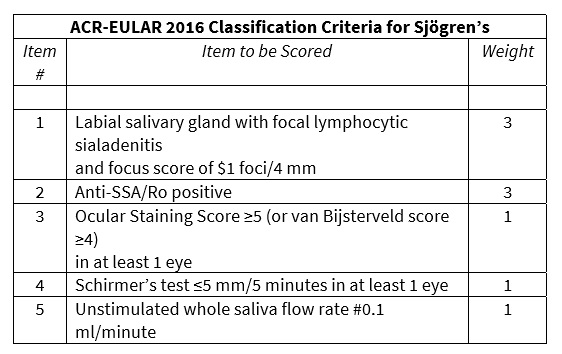
ACR-EULAR 2016 Classification Criteria for Sjögren’s for Clinical Trials:2-3
For a patient to be included in a clinical trial, diagnosis for any disease must meet very strict criteria. These criteria are called “Classification Criteria” and are NOT designed for diagnosis in the clinician’s office for management and treatment. With this caveat in mind, Classification Criteria can provide general guidance on diagnosis by providing clinicians with information about symptoms and tests that are clearly associated with a Sjögren’s diagnosis. Classification Criteria are updated as new tools are validated.
The most recent classification criteria for Sjögren’s were finalized in 2016 and approved by the American College of Rheumatology (ACR) Board of Directors and the European League Against Rheumatism (EULAR) Executive Committee. Criteria are based on the following:
- First, a patient must either be suspected of having Sjögren’s based on the EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI)3 with at least 1 domain being positive OR respond positively to at least one of the following questions about symptoms:
- Have you had daily, persistent, troublesome dry eyes for more than 3 months?
- Do you have a recurrent sensation of sand or gravel in the eyes?
- Do you use tear substitutes more than 3 times a day?
- Have you had a daily feeling of dry mouth for more than 3 months?
- Do you frequently drink liquids to aid in swallowing dry food?
- Second, a patient is excluded for any of the following:
- History of head and neck radiation treatment
- Active hepatitis C infection (with confirmation by polymerase chain reaction)
- AIDS
- Sarcoidosis
- Amyloidosis
- Graft-versus-host disease
- IgG4-related disease
- Finally, a diagnosis of Sjögren’s is based on the weighted sum of 5 items. A patient must have a total score of ≥4 to meet Classification Criteria for a Sjögren’s diagnosis for a clinical trial.
The criteria advise that patients taking anticholinergic drugs should be evaluated for objective signs of salivary hypofunction and ocular dryness only after being off these medications for a sufficient interval.
Until new tools are validated, such as the salivary gland ultrasound, and biomarkers are discovered that can further elucidate a diagnosis of Sjögren’s, most medical centers conducting clinical trials now will use the 2016 Classification Criteria for diagnosis. However, it is important to note that the previous version, the 2002 American-European Classification Criteria for Sjögren’s,5 have been used since their development for many clinical studies that continue to guide healthcare providers today. These criteria are slightly broader-based and weight oral and ocular symptoms more highly than the newer criteria.
References:
- Yokogawa N, Lieberman SM, Sherry DD, Vivino FB. Features of Childhood Sjögren's Syndrome in Comparison to Adult Sjögren's Syndrome: Considerations in Establishing Child-Specific Diagnostic Criteria. Clin Exp Rheumatol. 2016 Mar-Apr;34(2),343-51.
- Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, Rasmussen A, Scofield H, Vitali C, Bowman SJ, Mariette X, International Sjögren’s Syndrome Criteria Working Group. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren's Syndrome: A Consensus and Data-Driven Methodology Involving Three International Patient Cohorts. Arthritis Rheumatol. 2017 Jan;69(1),35-45.
- Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, Rasmussen A, Scofield H, Vitali C, Bowman SJ, Mariette X, International Sjögren’s Syndrome Criteria Working Group. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren's Syndrome: A Consensus and Data-Driven Methodology Involving Three International Patient Cohorts. Ann Rheum Dis. 2017 Jan;76(1)9-16.
- Seror R, Ravaud P, Bowman SJ, Baron G, Tzioufas A, Theander E, Gottenberg J-E, Bootsma H, Mariette X, Vitali C, EULAR Sjögren’s Task Force. Ann Rheum Dis. 2010 Jun;(6),1103-9.
- Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH, European Study Group on Classification Criteria for Sjögren’s Syndrome. Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002 Jun;61(6):554-8.